Artificial intelligence (AI) and Big Data are reshaping the healthcare landscape with potential implications that extend well beyond simple technological upgrades. These advancements have sparked significant interest and discussion, particularly in the field of cardiology, and they are emerging as pivotal tools for enhancing diagnostic precision, predicting disease onset, and personalizing treatment plans. A notable example is AI’s role in identifying conditions like atrial fibrillation (AFib), a common yet often asymptomatic heart condition. Such technological interventions promise not only to revolutionize heart health care by augmenting traditional diagnostic methods but also to democratize access to high-quality medical care. By deciphering vast amounts of health data to unearth patterns and trends, AI and Big Data are breaking new ground in healthcare, offering insights that promise to transform clinical practices and patient outcomes.
AI’s Role in Diagnostic Accuracy and Early Disease Detection
One profound benefit of AI in the realm of heart health is its potential to enhance the accuracy of diagnostics. Cases like that of Peter Maercklein, who was diagnosed with AFib through an AI-enabled algorithm, underscore this potential. Maercklein, who was asymptomatic, highlighted AI’s capacity to detect subtle changes in electrocardiograms (ECGs) that might be missed by human specialists. The Mayo Clinic’s adoption of AI-guided ECGs maximizes the diagnostic potential of a standard and cost-effective heart test. Precision diagnostics, as demonstrated by an 81.49% probability of AFib detection, pave the way for timely interventions in cardiovascular diseases, potentially altering the course of treatment for many patients.
Furthermore, the extensive data collected from wearable technology is becoming increasingly valuable in medical diagnostics. Devices like smartwatches continually gather health metrics which, when integrated with AI, can lead to the identification of emerging patterns indicative of underlying heart conditions. AI analyzes trends, offering predictions and insights that can foresee health issues even before symptoms manifest. Mayo Clinic’s development of an AI-ECG dashboard exemplifies this shift, integrating deep learning with patient health records to bolster diagnostic accuracy. It forecasts not only AFib but a spectrum of other cardiovascular conditions, enhancing clinicians’ ability to create informed, personalized care strategies. Such capabilities are fundamental in recognizing disease risk early, reducing the time from detection to treatment, and consequently improving patient outcomes.
Democratizing Access to Medical Diagnostics
The democratization of healthcare through advanced AI and Big Data tools is not just an aspirational goal; it is becoming a tangible reality. Historically, access to cutting-edge medical diagnostics has been restricted to those who can afford specialty care centers. AI, however, stands to level this playing field by offering accessible, cost-effective diagnostic solutions that do not necessitate proximity to a hospital or clinic. Algorithms developed for ECG interpretation are poised to enable initial screenings for heart diseases remotely, a boon for high-risk groups who need constant monitoring. Such technology also allows general practitioners to perform sophisticated tests once exclusively available at top-tier institutions.
Moreover, the simplification of advanced technical data into actionable insights for local healthcare providers exemplifies another layer of democratization. By implementing AI-driven tools in everyday healthcare practice, physicians can make data-informed decisions aligned with best practices, effectively eliminating systemic barriers to specialized care. As regulatory bodies review these diagnostic systems, their approval could catalyze a global transformation in heart disease management, making timely healthcare advances available to diverse populations irrespective of geography or economic status. The potential for widespread availability and cost reduction is significant, indicating a broader impact wherein technology empowers patients and doctors alike, facilitating earlier detection, more effective interventions, and enhanced overall health outcomes.
The Integration of Big Data in Healthcare
Big Data’s integration into healthcare is redefining the understanding of diseases and the development of treatments. It involves analyzing massive data sets to uncover trends and correlations that inform clinical decisions. The scope of Big Data encompasses diverse types and volumes of information, including electronic health records, social media inputs, and imaging data. Healthcare institutions like Mayo Clinic leverage this vast data pool to enhance research capabilities, identifying critical health insights that were previously unattainable. This data-centric approach offers the potential to predict disease patterns and patient responses to treatments, thus allowing for more nuanced, precise, and personalized healthcare solutions.
The analysis of such extensive datasets also provides insights into potential hazards associated with specific medications, exemplified by investigations like those conducted by the FDA. In examining rofecoxib (Vioxx), experts demonstrated the power of Big Data by analyzing 1.4 million patient records. This effort uncovered the drug’s linkage to increased heart attack risks, resulting in its market withdrawal. This case illustrates how modern data handling capabilities can generate substantial evidence quickly, supporting healthcare providers in making informed and timely decisions. As Big Data continues to permeate healthcare, the sector is expected to benefit from improved disease predictions, enhanced risk management, and novel therapeutic strategies, emphasizing prevention and efficiency in medical practices.
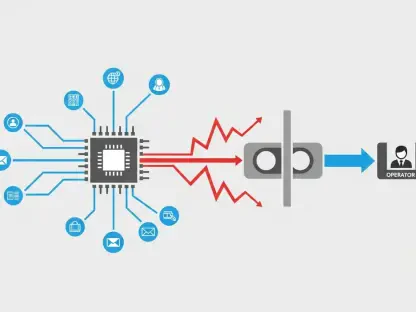
Distributed Computing and Data Analysis
The innovation brought about by distributed computing in processing Big Data stands as a cornerstone of modern healthcare analytics. Traditional data management systems would struggle under the burden of today’s expansive datasets, but distributed computing technologies allow multiple systems to function cohesively, regardless of their physical locations. This approach enhances computational capabilities, enabling complex analyses of both structured and unstructured data without prohibitive costs. Technologies like Hadoop support this transition by offering scalable storage solutions that align with the demands of contemporary healthcare information management.
As healthcare embraces these advancements, the focus is on uncovering intricate relationships between data points. For instance, distributed computing allows for the aggregation and interpretation of health trends, patient histories, and environmental factors in combination. This holistic view bolsters the identification of patterns that constitute early preventive measures or tailored interventions. The capability to process large datasets efficiently provides healthcare professionals with a comprehensive toolkit for predicting patient trajectories and outcomes. The intersection of AI and Big Data, underpinned by robust computing foundations, leads to an unprecedented understanding of health indicators, ultimately supporting proactive, evidence-based medical pathways that prioritize patient-centric care.
Bridging Technology and Healthcare Accessibility
The crucial link between AI, Big Data, and expanded healthcare accessibility reinforces the commitment to a more uniform distribution of health benefits across various communities. By leveraging advanced technologies, healthcare providers aim to address disparities that have long characterized medical care distribution. AI and Big Data are instrumental in crafting solutions that cater to the specific needs of underserved and remote populations, thereby fostering inclusivity in healthcare provision.
Efforts to bridge technology and accessibility focus on deploying portable diagnostic tools and mobile health applications designed to work in tandem with existing healthcare systems. These innovations offer real-time monitoring and feedback, empowering patients to take a proactive stance toward their health management. Additionally, AI confidently interprets diverse diagnostic outputs, ensuring that healthcare services are both cost-efficient and replicable across different settings. This approach decreases reliance on centralized healthcare facilities and encourages the development of sustainable care models that adapt to various demographic and infrastructural constraints.
From policy adjustments to community engagement frameworks, technology’s role in enhancing healthcare accessibility underscores the broader vision of equitable care. The ongoing dialogue around best practices emphasizes creating regulatory avenues that facilitate the seamless integration of these tech-driven solutions into public health systems. As AI and Big Data technologies gain traction, their ability to adapt and respond to real-time challenges will likely be central to overcoming existing healthcare inequities and achieving comprehensive patient care.
Future Implications and Impact on Healthcare Systems
As AI and Big Data continue to evolve, the implications for healthcare systems are profound and multifaceted. These technologies promise not only to consolidate diagnostic precision and treatment efficacy but also to redefine healthcare delivery models. By emphasizing predictive analytics, healthcare can move towards a more preventative rather than reactive care approach, reshaping patient interaction frameworks and healthcare infrastructure management. The shift towards technology-driven care aligns with the global push for value-based healthcare, where outcomes are optimized, and resources are utilized efficiently.
The anticipated widespread adoption of these innovations presents a host of challenges and opportunities for stakeholders across the healthcare continuum. Training and education for healthcare professionals will be essential to harness the full potential of AI and Big Data, requiring an interdisciplinary approach that combines clinical expertise with data-centric skills. Policymakers and healthcare administrators must navigate issues related to data privacy and security, establishing ethical guidelines that uphold patient confidentiality while fostering technological advancement.
Moreover, as regulatory procedures evolve to accommodate these emerging technologies, healthcare systems have the potential to transform fundamentally, ensuring real-time insights drive patient care decisions. The integration of AI and Big Data and the collaborative effort across sectors will be instrumental in shaping resilient healthcare frameworks that are adaptable to future innovations and challenges.
Transformative Pathways for Global Health
Artificial intelligence (AI) is revolutionizing heart health diagnostics, offering enhanced accuracy in identifying cardiovascular issues. A prime example is Peter Maercklein’s diagnosis of atrial fibrillation (AFib) using an AI-driven algorithm. Despite showing no symptoms, Maercklein benefited from AI’s ability to spot subtle changes in electrocardiograms (ECGs) that might elude human specialists. Mayo Clinic has embraced AI to optimize ECG use, turning this routine heart test into a robust diagnostic tool. Thanks to AI precision, the likelihood of detecting AFib was remarkably high at 81.49%, enabling prompt intervention that could change treatment paths for numerous patients.
Wearable technology is also transforming medical diagnostics by providing a steady stream of valuable health data. Devices like smartwatches monitor essential health metrics, and when paired with AI, they help uncover trends indicative of potential heart issues. AI evaluates these patterns, predicting health concerns even before symptoms arise. Mayo Clinic’s AI-ECG dashboard is a testament to this advancement, combining deep learning with patient records to improve diagnostic precision. It forecasts not just AFib but a range of cardiovascular conditions, aiding clinicians in developing personalized care plans. These tools are crucial for early disease detection, reducing the gap between diagnosis and treatment, ultimately leading to better patient outcomes.