In the fast-paced and increasingly intricate realm of clinical research, the mounting challenges of managing vast data sets, accelerating timelines, and engaging diverse patient populations are driving a significant shift in approach. Pragmatic innovation, characterized by practical and value-focused strategies, is rapidly becoming a cornerstone of modern clinical trials, offering solutions that streamline processes while maintaining rigorous standards. This transformation is not merely a passing trend but a critical adaptation to the complexities of today’s research environment, where traditional methods often fall short. Global clinical data leaders from key hubs such as Basel, New York, London, and Copenhagen are converging on a shared vision of simplifying and standardizing practices. Their collective efforts aim to enhance efficiency, improve data quality, and prioritize patient needs, ensuring that clinical trials deliver meaningful outcomes for sponsors, regulators, and participants alike. This movement represents a pivotal moment for the industry, setting the stage for a more agile and impactful future.
Addressing Complexity with Practical Solutions
The clinical trial landscape has grown exponentially complex, with an overwhelming influx of data from diverse sources rendering outdated methods like comprehensive source data verification (SDV) impractical. Pragmatic innovation offers a remedy through risk-based quality management (RBQM), a strategy that targets critical risks rather than scrutinizing every data point. By leveraging advanced technology, this approach significantly reduces manual effort, as demonstrated by major biopharma companies that have cut thousands of hours of work for clinical research associates. The result is not only a boost in operational efficiency but also a sharper focus on data integrity where it matters most, allowing trials to progress without unnecessary delays. This shift underscores a broader recognition that sustainable practices must replace labor-intensive traditions to keep pace with the demands of modern research.
Beyond data challenges, the urgency to shorten trial timelines and expand patient access has intensified. Regulatory bodies, notably the FDA, are advocating for pragmatic trial designs that align closely with real-world clinical settings. Such designs facilitate faster research cycles by simplifying protocols and integrating real-life scenarios into study frameworks. Moreover, they promote inclusivity by accommodating a wider range of participants, ensuring that trial results are more representative of actual patient experiences. This regulatory support validates the industry’s pivot toward practicality, reinforcing the notion that clinical trials must evolve to address both scientific and societal needs effectively. The emphasis on mirroring routine care highlights a fundamental change in how trials are conceptualized and executed.
Harnessing Technology for Smarter Research
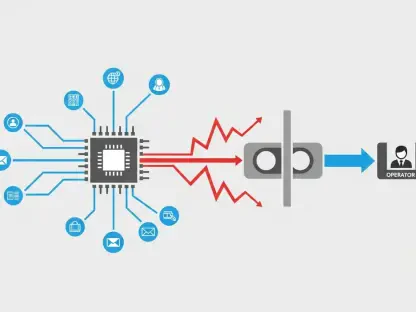
Technology stands as a linchpin in the pragmatic innovation movement, particularly through the transition from conventional data management to a data science paradigm. This evolution involves moving past mere data collection and cleaning to extracting actionable insights using tools like artificial intelligence (AI) and machine learning (ML). Clinical leaders are redefining team roles, emphasizing analytical skills over repetitive tasks, and equipping staff to anticipate trends and outcomes. This forward-thinking approach enables more informed decision-making, transforming raw data into strategic assets that drive trial success. However, the journey requires robust data foundations and cross-functional collaboration to ensure that technological advancements yield consistent, reliable results across varied contexts.
Another technological breakthrough is the adoption of smart automation, which integrates rule-based systems with cutting-edge AI to optimize data handling. Unlike uniform automation models, this tailored method selects the most effective technique for each specific task, accelerating processes like data cleaning while establishing a framework for future innovations such as fraud detection or compliance forecasting. The immediate advantages include enhanced efficiency and heightened trust in data accuracy, though challenges persist in defining universal performance metrics across diverse teams and studies. Smart automation exemplifies how technology can balance short-term gains with long-term potential, providing a scalable solution that adapts to the evolving needs of clinical research.
Streamlining Standards for Faster Outcomes
Standardizing data practices is a vital component of pragmatic innovation, yet clinical leaders are adopting a more focused strategy to avoid past pitfalls. Rather than attempting to consolidate all data into a single, unwieldy metadata repository (MDR), the emphasis is now on prioritizing essential study design elements. This refined approach accelerates trial setup and database finalization, ensuring that studies move forward swiftly without compromising on quality. By concentrating efforts on critical metadata, the industry sidesteps the delays often associated with overambitious centralization projects, demonstrating a practical mindset that values speed and precision over unnecessary complexity. This targeted standardization is proving to be a game-changer in maintaining momentum throughout the trial lifecycle.
The benefits of streamlined standards extend to operational agility, enabling research teams to adapt quickly to changing requirements or unexpected hurdles. Focused MDR strategies reduce the administrative burden, freeing up resources for innovation and problem-solving. Additionally, this method fosters consistency across studies, making it easier to compare results and draw meaningful conclusions. As clinical trials grow in scope and diversity, having a clear, manageable framework for data standards ensures that researchers can maintain high standards without getting bogged down by logistical challenges. This balance between structure and flexibility is essential for sustaining progress in an increasingly dynamic field.
Prioritizing Patient Engagement and Choice
At the core of pragmatic innovation lies a renewed commitment to patient-centricity, particularly through the concept of patient optionality. Instead of fixating on whether trials should be fully decentralized or site-based, the focus has shifted to offering participants flexible choices—whether to engage from home, a local clinic, or a dedicated research facility. This adaptability addresses the alarmingly low participation rates, with only about 3% of U.S. physicians and patients currently involved in trials, a factor contributing to delays in nearly 80% of studies. By tailoring participation methods to individual preferences, the industry aims to dismantle barriers, making trials more accessible and appealing to a broader demographic, ultimately enhancing enrollment and retention rates.
Reducing the burden on participants is equally critical to this patient-first approach. Thoughtful protocol designs that limit unnecessary data collection, combined with policies like “bring your own device” (BYOD) for data submission, prioritize convenience and security. These measures not only make participation less daunting but also build trust by respecting patient autonomy and privacy. The ripple effect is significant—engaged patients are more likely to remain committed to trials, providing richer, more reliable data. As the industry refines these strategies, the goal is to create a seamless trial experience that feels less like a clinical obligation and more like a collaborative health journey, fundamentally reshaping how patients interact with research.
Regulatory Alignment Paves the Way Forward
Regulatory endorsement is providing a crucial boost to pragmatic innovation, with the FDA’s recent guidance on pragmatic clinical trials signaling strong support for industry shifts. By advocating for study designs that reflect everyday clinical care, regulators are ensuring that research outcomes are more applicable to real-world scenarios. This alignment encourages the inclusion of diverse populations often underrepresented in traditional trials, addressing long-standing gaps in data relevance. The result is a framework where scientific rigor meets practical utility, allowing trials to serve both research objectives and the immediate needs of healthcare systems, ultimately benefiting a wider array of patients.
This regulatory backing also instills confidence among stakeholders, validating the move toward efficiency-driven and patient-focused methodologies. It prompts clinical leaders to refine protocols in ways that balance speed with quality, ensuring that accelerated timelines do not undermine data integrity. As the industry continues to align with these guidelines, the expectation is that trials will become more agile and inclusive, breaking down historical barriers to participation. Looking back, the strides made through this regulatory harmony marked a turning point, setting a precedent for how clinical research adapted to meet contemporary demands with clarity and purpose.
Building on Past Progress for Future Success
Reflecting on the journey, the embrace of pragmatic innovation fundamentally altered the trajectory of clinical trials, addressing inefficiencies that once hindered progress. The adoption of risk-based quality management, data science, smart automation, focused data standards, and patient optionality collectively redefined industry standards. These efforts tackled longstanding issues like low enrollment and cumbersome processes, laying a solid foundation for more responsive research models. Moving forward, stakeholders should continue to invest in scalable technologies and training to sustain this momentum. Additionally, fostering stronger collaborations between researchers, regulators, and patients will ensure that future trials remain both innovative and grounded in real-world needs. Prioritizing actionable strategies over rigid traditions will be key to navigating upcoming challenges, ensuring that clinical research not only keeps pace with complexity but also drives meaningful health advancements.