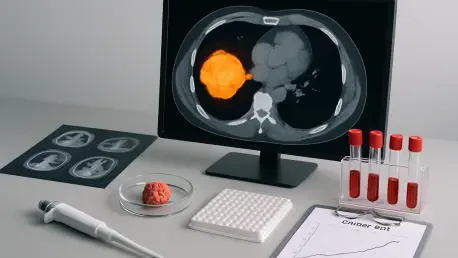
Imagine a world where leukemia, a devastating group of blood cancers impacting countless individuals globally, is no longer approached with a generic treatment plan but with a strategy meticulously tailored to each patient’s unique profile, offering hope for better outcomes. Predictive models, innovative tools designed to anticipate disease progression and therapeutic outcomes, stand poised to revolutionize this landscape. By harnessing extensive data—from genetic markers to detailed clinical histories—these models aim to equip physicians with the insights needed to make more informed, impactful decisions. The potential to shift from broad, standardized care to precise, individualized interventions is within reach, offering renewed hope for better survival rates and improved quality of life. As leukemia encompasses diverse subtypes like acute myeloid leukemia (AML) and chronic lymphocytic leukemia (CLL), each with distinct behaviors and challenges, the urgency for such tailored approaches becomes even clearer. This exploration delves into how predictive models could redefine the fight against this complex disease.
Navigating the Challenges of Current Predictive Tools
The promise of predictive models in leukemia care is immense, yet their current landscape reveals significant obstacles that must be addressed. Many existing tools exhibit inconsistent accuracy, often stemming from variations in development methodologies or insufficient testing across diverse patient cohorts. This inconsistency raises critical questions about their reliability in real-world clinical environments. Without robust validation, there’s a risk that these models might deliver misleading predictions, potentially affecting treatment decisions. The need for standardized testing protocols is evident, as is the push to ensure these tools are applicable to a broader range of patients, regardless of demographic or geographic differences. Overcoming these hurdles is essential to build trust in predictive technologies and to ensure they can be seamlessly integrated into everyday medical practice, ultimately benefiting those battling various forms of leukemia.
Another pressing concern lies in the incomplete scope of many predictive models. Often, these tools fail to account for crucial biological factors such as genetic mutations or the specific microenvironment surrounding leukemia cells, both of which heavily influence disease progression and response to therapy. Additionally, external elements like lifestyle choices or socioeconomic conditions are frequently overlooked, despite their impact on overall health outcomes. Researchers are increasingly advocating for a more holistic approach, urging the development of models that capture a fuller spectrum of influences on a patient’s condition. By addressing these gaps, predictive tools could offer a more accurate and comprehensive view, enabling clinicians to design interventions that are not only more effective but also more aligned with the intricate realities of each patient’s life and disease profile.
Harnessing Technology for Precision in Prediction
The integration of advanced technologies like machine learning and big data analytics marks a transformative era for predictive modeling in leukemia treatment. These powerful tools excel at sifting through enormous datasets to identify subtle patterns and correlations that traditional statistical methods might miss. By refining predictions to an individual level, they hold the potential to accelerate diagnoses and inform highly personalized treatment plans. The excitement surrounding this capability is well-founded, as it could lead to earlier interventions and more targeted therapies, significantly enhancing patient outcomes. As these technologies continue to evolve, their ability to handle complex, multidimensional data offers a glimpse into a future where leukemia care is far more precise and effective, tailored to the unique genetic and clinical makeup of each patient.
However, translating these technological advancements into practical clinical tools presents notable challenges. The inherent complexity of machine learning algorithms often conflicts with the need for straightforward, interpretable solutions that healthcare providers can readily adopt. If these models are to make a tangible impact, they must be designed with usability in mind, ensuring that physicians can understand and apply their insights without requiring extensive technical expertise. This necessitates close collaboration between computational scientists and clinical oncologists to bridge the gap between innovation and application. Such partnerships are vital to ensure that technological breakthroughs do not remain confined to research labs but are effectively woven into the fabric of daily medical practice, ultimately improving the way leukemia is managed across diverse healthcare settings.
Improving Risk Stratification and Ensuring Fairness
One of the most compelling advantages of advanced predictive models is their potential to enhance risk stratification in leukemia care. This process involves identifying which patients face a higher likelihood of rapid disease progression, allowing clinicians to prioritize aggressive treatments for those in greatest need while sparing others from unnecessary, harsh therapies. Improved models could provide clearer insights into individual risk profiles, enabling a more nuanced approach to treatment planning. This targeted strategy not only has the potential to boost survival rates but also to reduce the burden of side effects, ensuring that patients receive care that is both effective and considerate of their overall well-being. As research progresses, the refinement of risk assessment tools stands out as a critical step toward optimizing outcomes in the management of this challenging disease.
Equally important is the pressing need to address equity in the development of predictive models. A significant limitation of many current tools is their reliance on data from narrow demographic groups, which can lead to biased predictions that fail to serve diverse populations effectively. This lack of inclusivity raises serious concerns about fairness and the universal applicability of these technologies. To counter this, future research must prioritize inclusive study designs that reflect a wide range of ethnic, geographic, and socioeconomic backgrounds. By ensuring that predictive models are tested and validated across varied cohorts, the medical community can work toward equitable access to cutting-edge care, guaranteeing that the benefits of technological advancements in leukemia treatment are shared by all patients, regardless of their personal circumstances or location.
Paving the Way for Future Innovations
Reflecting on the journey of predictive modeling in leukemia care, it’s evident that significant strides have been made in identifying both the immense potential and the persistent shortcomings of these tools. The exploration of their capacity to personalize treatment, driven by insights from machine learning and comprehensive data integration, marked a pivotal moment in oncology. Efforts to address inconsistencies in accuracy and the lack of diversity in testing have been central to discussions, as was the emphasis on interdisciplinary collaboration to ensure practical application. These past endeavors laid crucial groundwork, highlighting the importance of continuous improvement and adaptation in the face of complex clinical challenges.
Looking ahead, the path forward involves actionable steps to refine and expand the reach of predictive models. Prioritizing rigorous validation processes and fostering inclusive research are essential to eliminate biases and enhance reliability. Additionally, investing in clinician training programs will ensure that healthcare providers are well-equipped to interpret and utilize these advanced tools effectively. By focusing on these initiatives, the medical field can move closer to a future where leukemia treatment is not only more precise but also universally accessible, offering renewed hope and improved care for patients worldwide.