Healthcare systems have struggled to anticipate risk hidden in disconnected records, but the new reality is that predictive platforms can surface looming problems fast enough to change outcomes, budgets, and trust. Instead of waiting for claims to settle or quarterly reports to land, care teams can receive timely signals about rising risk, administrators can steer resources before bottlenecks form, and payers can align incentives with outcomes rather than volume. The pivot sounds technical, yet it is fundamentally organizational: it depends on unifying data across entities, ensuring fairness in models, and fitting insights into the minute-by-minute flow of clinical work. When those pieces come together, the promises of value-based care move from PowerPoint to practice, and population health strategies finally take root.
From Retrospective to Predictive Care
The shift from retrospective analysis to real-time prediction marked a break with decades of looking back at utilization and cost trends, then guessing what to do next. Machine learning models now forecast hospitalization risk, disease progression, and medication gaps days or weeks ahead, giving care teams a chance to intervene with targeted outreach, virtual visits, or medication adjustments. Crucially, the impact stems from embedding these predictions in the workflow, not from generating another dashboard. Prioritized task lists, alert thresholds tuned to clinical context, and clear accountability allow clinicians to move from passive monitoring to decisive action, reducing avoidable acute events and improving continuity.
Moreover, predictive programs have reframed care planning as a continuous process rather than a series of episodic check-ins. When algorithms update risk profiles as new vitals, lab results, or pharmacy fills arrive, care teams can adjust plans in step with the patient’s status, not weeks later. The most effective implementations pair risk flags with recommended next steps calibrated to resources: a social worker referral if food insecurity is detected, a pharmacist review when adherence dips, or home health after early deconditioning appears. This translation from forecast to feasible action has proven decisive, turning probabilities into practical improvements measured in fewer readmissions and steadier chronic disease control.
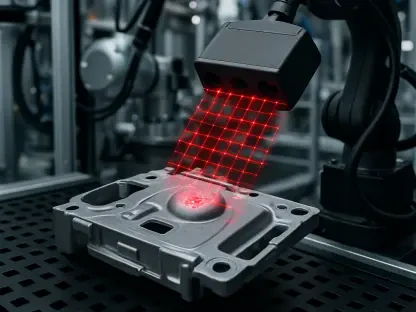
Data Integration and Real-Time Intelligence
The predictive turn depends on data breadth as much as model sophistication. Platforms that harmonize electronic health records, claims, social determinants, and wearable signals build a richer view of risk than any single source can supply. Standardized data models and APIs reduce the friction of pulling information from disparate systems, translating varied coding schemes into a common language that analytics can understand. With that foundation, models can examine clinical trajectories, benefit design, care access, and environmental exposures together, detecting patterns—like seasonal exacerbations layered on transportation gaps—that would remain invisible in siloed views.
In practice, this integration has enabled more granular risk stratification and better forecasts of utilization. Instead of broad labels such as “high risk,” platforms infer probable needs at a service-line level: cardiology follow-up within seven days, behavioral health engagement within thirty, or an adherence check based on refill irregularities. Streaming data from wearables adds context on activity and sleep, while neighborhood indicators capture heat, air quality, and food access. These inputs do not replace clinician judgment; they refine it. When surfaced through intuitive summaries and concise narratives, the intelligence nudges teams toward timely, appropriate interventions that respect both clinical nuance and patient preferences.
Enabling Value-Based Models
Value-based care requires timely insight into risk, performance, and cost drivers, and AI platforms have supplied the common signals that providers and payers long sought. Real-time attribution and risk adjustment reduce the lag between service delivery and financial accountability, shrinking the guesswork that erodes margins and morale. Performance benchmarking based on current clinical and utilization trends, rather than claims from months past, allows contract managers to steer mid-year, correcting course before losses lock in. The outcome is more precise shared savings calculations and fewer disputes about data provenance or methodology.
Just as important, these tools have helped align incentives around prevention and coordination. When both parties see the same up-to-date risk profiles and care gap lists, it becomes easier to fund care navigation, home visits, and community partnerships that avert costly episodes. Contract terms can reward early interventions documented through the platform—such as adherence outreach or post-discharge checks—tying payments to actions, not just endpoints. Over time, this clarity has supported a more collaborative posture in negotiations, as stakeholders use common evidence to shape benefit designs, network configurations, and care pathways that make quality and affordability mutually achievable.
Operational and Financial Optimization
Operational leaders have leaned on predictive intelligence to smooth patient flow, anticipating bottlenecks and calibrating resources in advance. Demand forecasts inform staffing for nursing units, clinics, and specialty services, while bed and discharge predictions guide surge planning and weekend coverage. Emergency departments use arrival and acuity forecasts to optimize triage and fast-track protocols, reducing wait times and diversions. When models highlight patients likely to face discharge barriers, case managers can mobilize transport, equipment, or home services early, shortening length of stay without compromising safety. These interventions accumulate into steadier throughput and less burnout.
Financially, linking clinical risk with utilization and claims has illuminated cost drivers with unusual clarity. Rather than chasing global cost targets, organizations can pinpoint cohorts with outsized avoidable spend and match them to specific interventions: medication therapy management for polypharmacy, intensive case management for frequent ED users, or remote monitoring for heart failure. Payers use the same intelligence for risk-adjusted payments and real-time oversight of contract performance, tamping down volatility. What previously felt like financial whiplash has become manageable variance, as targeted programs are monitored for effect size and refined pragmatically, keeping quality steady while bending total cost of care.
Equity, Public Health, and Research
Incorporating social and environmental factors changed the equity conversation from aspiration to execution. Platforms flag needs related to housing instability, food access, transportation, or language, guiding resource allocation toward those most at risk of falling through the cracks. Outreach campaigns can be tailored for cultural relevance and delivered through trusted community partners, while closed-loop referrals verify that social services were actually received. Public health teams gain a window into neighborhood-level patterns, spotting clusters of chronic disease complications or vaccination gaps and adjusting programs accordingly, with clearer accountability for impact.
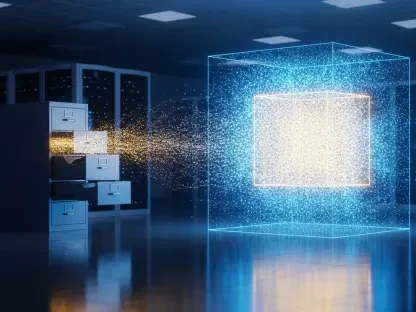
Beyond immediate operations, de-identified, population-level datasets have supported research on care patterns, treatment effectiveness, and the influence of social determinants. These studies feed into guidelines and policy, helping standard-setters update quality measures and coverage criteria with real-world evidence. Integrating environmental data—heat waves, wildfire smoke, pollen counts—has sharpened predictive models for exacerbations and hospital demand. The same evidence base informs city and state planning, from cooling centers to transportation subsidies, linking clinical predictions to community action. The result is a tighter loop between insight, intervention, and policy that makes equity measurable and progress durable.
Trust, Usability, and Governance Challenges
Adoption has hinged on trust built through explainability, usability, and governance rather than performance metrics alone. Clinicians asked for clear reasons behind risk scores and concise summaries of the top drivers, not probabilistic jargon. Interfaces that surface patient context, past interventions, and recommended actions have outperformed black-box alerts that erode confidence. Embedding decision support in existing EHR workflows, minimizing duplicate clicks, and aligning notifications with clinical priority reduced alert fatigue. Where platforms delivered reliable, interpretable guidance at the right moment, staff engagement rose and outcomes followed.
Governance proved equally central. Responsible AI programs established fairness metrics up front, audited models for bias drift, and retrained with broader, more representative datasets. Privacy-first architectures applied de-identification when appropriate, end-to-end encryption, and rigorous role-based access controls, with compliance checks baked into each step of the data lifecycle. Importantly, cross-functional committees—clinicians, data scientists, compliance officers, and community representatives—set guardrails on acceptable use and escalation paths for issues. This structure balanced innovation with accountability, sustaining trust while allowing rapid iteration when workflows or regulations changed.
Design Trade-Offs and Implementation Pathways
Implementation required navigating trade-offs without losing sight of outcomes. Standardization enabled interoperability, yet models needed local tuning to reflect demographics, practice patterns, and resource realities. Explainability improved trust, but oversimplification risked misleading users; the answer lay in layered transparency that offered plain-language rationales with optional detail. Most of all, prediction meant little without operationalization. Winning programs translated insights into accountable actions: who does what, by when, with what documentation, and how impact is measured. That rigor turned analytics from interesting to indispensable.
Looking ahead, durable progress depended on three practical steps that had already proved their value. First, build for interoperability with standardized data models and robust APIs so signals flow across settings without handoffs failing. Second, embed responsible AI from the outset—fairness audits, continuous monitoring, and privacy-by-design—so models adapt safely as populations and practices evolve. Third, close the loop between prediction and service delivery by integrating tasking, referral management, and outcome tracking, ensuring investments in navigation, adherence support, and community services translate into measurable gains. Taken together, these pathways had positioned predictive platforms as essential infrastructure for equitable, sustainable care.